Phospholipid and antiphospholipid syndrome
Time:2025-05-19Antiphospholipid syndrome (APS) is an autoimmune disease characterized by recurrent arterial or venous thrombosis, morbid pregnancy, and persistent positivity of antiphospholipid antibodies. Phospholipids are of great significance in the pathogenesis, clinical manifestations, diagnosis, and treatment of antiphospholipid syndrome, which are introduced in detail as follows:
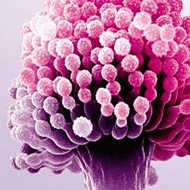
I. Overview of Phospholipids
Phospholipids, a class of lipids containing phosphoric acid, are important components of biological membranes and play a key role in maintaining cellular structure and function. Common phospholipids include phosphatidylcholine, phosphatidylethanolamine, phosphatidylserine, etc., which are widely present in human cell membranes, plasma lipoproteins, and other structures.
II. Phospholipids and Pathogenesis of Antiphospholipid Syndrome
1. Production of Autoantibodies
In APS patients, the immune system mistakenly recognizes phospholipids or phospholipid-bound proteins as foreign antigens, generating autoantibodies against them, namely antiphospholipid antibodies. These antibodies mainly include lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-β₂-glycoprotein I antibodies (anti-β₂-GPⅠ).
2. Mechanism of Thrombosis
Vascular Endothelial Damage
Antiphospholipid antibodies bind to phospholipids on the surface of vascular endothelial cells, activating the endothelial cells and increasing their expression of adhesion molecules, which attract inflammatory cells to accumulate, leading to damage and dysfunction of vascular endothelial cells. Damaged endothelial cells release procoagulant substances such as tissue factor, activating the coagulation system and promoting thrombosis.
Platelet Activation
Antiphospholipid antibodies bind to phospholipids on the platelet membrane, causing platelet activation and aggregation, and releasing platelet factors, which further enhance the coagulation response and accelerate thrombus formation and development.
Imbalance of Coagulation-Anticoagulation System
Antiphospholipid antibodies disrupt the coagulation-anticoagulation balance in the body. On the one hand, they inhibit the activity of anticoagulant substances such as protein C and protein S; on the other hand, they promote the activation and release of coagulation factors, leading to a hypercoagulable state of the blood and facilitating thrombosis.
3. Mechanism of Morbid Pregnancy
Placental Vascular Lesions
Antiphospholipid antibodies deposit in the placental vascular wall, causing damage to placental vascular endothelial cells and thrombosis, leading to insufficient placental blood supply. This affects the supply of nutrients and oxygen to the fetus, resulting in fetal growth restriction, fetal demise, miscarriage, and other morbid pregnancy outcomes.
Immune Damage
Antiphospholipid antibodies may also trigger immune attacks on placental tissues by activating the maternal immune system, disrupting the normal structure and function of the placenta.
III. Clinical Manifestations of Antiphospholipid Syndrome
1. Thrombosis
Thrombosis can occur in arteries or veins. Arterial thrombosis commonly occurs in the brain, leading to cerebral infarction with symptoms such as headache, hemiplegia, and aphasia; it can also occur in the coronary arteries, causing myocardial infarction with manifestations such as chest pain and palpitations. Venous thrombosis most commonly involves the deep veins of the lower extremities, presenting as lower limb swelling, pain, and exacerbation after activity.
2. Morbid Pregnancy
This includes habitual abortion, embryonic arrest, fetal growth restriction, preeclampsia or eclampsia, and placental insufficiency. These manifestations usually occur in the second or third trimester of pregnancy and seriously affect the health of both the mother and the fetus.
3. Other Manifestations
Some patients may also experience thrombocytopenia, manifested as petechiae, ecchymoses, epistaxis, gum bleeding, etc.; joint pain and swelling similar to rheumatoid arthritis; as well as livedo reticularis and valvular lesions.
IV. Diagnosis
1. Clinical Manifestations
Doctors will thoroughly understand the patient's medical history, including a history of thrombosis (such as cerebral infarction, myocardial infarction, deep vein thrombosis, etc.), a history of morbid pregnancy (such as multiple abortions, fetal arrest, etc.), and the presence of symptoms such as thrombocytopenia and livedo reticularis.
2. Laboratory Tests
Detection of antiphospholipid antibodies is key to diagnosing antiphospholipid syndrome. Common test items include lupus anticoagulant, anticardiolipin antibodies, and anti-β₂-glycoprotein I antibodies. Generally, positive results in at least two tests separated by 12 weeks, combined with clinical manifestations, are required for a definite diagnosis.
V. Treatment
1. Anticoagulant Therapy
This is the core of APS treatment. Commonly used drugs include warfarin and low-molecular-weight heparin (LMWH). Warfarin exerts anticoagulant effects by inhibiting the synthesis of vitamin K-dependent coagulation factors but requires regular monitoring of the international normalized ratio (INR) to adjust the drug dose, maintaining INR between 2 and 3. LMWH has the advantages of good anticoagulant effect and relatively low bleeding risk, and is often used for anticoagulant treatment in pregnant patients.
2. Immunosuppressive Therapy
For patients with severe disease or those combined with other autoimmune diseases, glucocorticoids (such as prednisone) and immunosuppressants (such as cyclophosphamide, azathioprine, etc.) may be used to inhibit abnormal immune responses and reduce the production of antiphospholipid antibodies.
3. Other Treatments
For patients with thrombocytopenia, drugs such as glucocorticoids and immunoglobulin can be used to increase platelet count; for patients at high risk of thrombosis, prophylactic anticoagulant measures can be taken.


 CN
CN