Phospholipids in pharmaceutical preparations
Time:2025-05-26I. Phospholipids as Core Carriers in Drug Delivery Systems
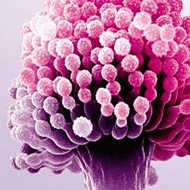
The amphiphilic molecular structure of phospholipids (such as lecithin and synthetic phospholipids) makes them natural nanocarrier skeletons, forming various delivery systems through self-assembly. Core advantages include:
Biomembrane compatibility: Phospholipid bilayers resemble cell membranes, reducing immune rejection and enhancing cellular uptake efficiency.
Drug-loading flexibility: Hydrophilic lumens (for water-soluble drugs) and hydrophobic layers (for lipid-soluble drugs) enable biphasic drug loading. For example, paclitaxel-phospholipid complexes achieve a drug loading of 30% (w/w).
Controllable metabolism: Natural phospholipids are gradually degraded by endogenous phospholipases, avoiding long-term accumulation toxicity.
II. Technological Breakthroughs in Innovative Delivery Systems
1. Environment-Responsive Design of Intelligent Liposomes
pH-sensitive liposomes: Phospholipids modified with oleic acid (e.g., DODAC) dissociate lipid bilayers in the tumor microenvironment (pH 6.0–6.5), accelerating drug release. For instance, pH-sensitive doxorubicin liposomes exhibit 2.3-fold higher tumor accumulation and 40% lower cardiac toxicity than conventional liposomes in tumor-bearing mice.
Temperature-sensitive liposomes: Blending dipalmitoyl phosphatidylcholine (DPPC) with myristoyl phospholipids creates liposomes with a phase transition temperature (42°C) close to tumor hyperthermia temperatures. Local hyperthermia triggers rapid drug release in tumors, increasing paclitaxel concentration 3-fold in tumors and reducing normal tissue distribution by 50% in mouse models.
2. Upgraded Applications of Nanostructured Lipid Carriers (NLC)
Phospholipid-solid lipid composite skeletons: NLC with 100–200 nm particle size prepared by mixing glyceryl stearate (solid lipid) and lecithin at 3:1 ratio. For oral insulin delivery, phospholipid interactions with intestinal mucosa increase insulin absorption from 5% to 18%, extending plasma concentration maintenance to 8 hours (vs. 4 hours for traditional formulations).
Targeted delivery of surface-modified NLC: Grafting phospholipid-targeting peptides (e.g., RGD peptide) onto NLC constructs a "phospholipid-peptide-drug" ternary system. Animal experiments show 4.7-fold higher lung cancer cell targeting efficiency and 3-fold increased intracellular doxorubicin uptake compared to unmodified NLC.
3. Functional Expansion of Self-Assembled Nanomicelles
Amphiphilic phospholipid-polymer conjugate systems: Covalently linking methoxy polyethylene glycol (mPEG) to phosphatidylethanolamine (PE) (mPEG-PE) forms 50–80 nm micelles. Encapsulating insoluble drugs (e.g., curcumin) achieves 15% drug loading, extends blood circulation half-life from 0.5 to 6 hours, and increases liver-targeted accumulation by 2.5-fold.
Light-responsive phospholipid micelles: Introducing azobenzene-modified phospholipids causes micelle structure disruption and drug release under UV light (365 nm), as azobenzene converts from trans to cis conformation. For local skin cancer treatment, this system releases 80% of the drug within 5 minutes of irradiation, versus only 20% over 24 hours without light.
III. Innovative Applications of Phospholipids in Oral Delivery Systems
1. Construction of Enteric-Coated Phospholipid Microcapsules
Multilayer phospholipid-cellulose composite microcapsules: Lecithin-core microcapsules (500–1000 μm diameter) coated with hydroxypropyl methylcellulose phthalate (HPMCP). For oral protein drugs (e.g., growth hormone), microcapsules maintain >90% integrity in gastric acid, and phospholipase degradation of lecithin triggers drug release in the intestine, increasing bioavailability from <1% to 8%.
2. Optimization of Self-Emulsifying Drug Delivery Systems (SMEDDS)
Phospholipid-medium-chain triglyceride (MCT) synergistic systems: Soy lecithin-MCT blends (1:2) form O/W emulsions (particle size <50 nm) upon contact with water. For example, cyclosporine SMEDDS exhibits 1.8-fold higher oral bioavailability than commercial capsules, with 30% improved absorption stability during meals (traditional formulations are diet-sensitive).
3. Mucoadhesive Phospholipid Nanoparticles
Chitosan-phospholipid conjugate nanoparticles: 200 nm nanoparticles formed by electrostatic interaction between cationic chitosan and anionic phospholipid nanoparticles. For nasal administration, mucoadhesion time extends from 2 to 8 hours, enhancing brain-targeted insulin delivery by 3-fold and prolonging blood glucose control to 12 hours in diabetic mice.
IV. Phospholipid Strategies for Local Delivery and Targeted Therapy
1. Innovative Permeation-Enhancing Mechanisms for Transdermal Delivery
Phospholipid ethosomes for permeation enhancement: Adding ethanol (20%–40%) to phospholipid-drug systems forms flexible vesicles. For psoriasis treatment, tazarotene skin permeability increases 5-fold compared to ordinary liposomes, with 3-fold higher stratum corneum accumulation and reduced systemic toxicity (plasma drug concentration decreases 60%).
Microneedle-phospholipid composite delivery systems: Coating phospholipid-drug layers (5–10 μm thickness) on solid microneedles fuses with stratum corneum lipids during skin puncture, promoting drug penetration. Experiments show insulin microneedle-phospholipid coatings reduce blood glucose 1.5 hours faster than subcutaneous injection with 30% lower dosage.
2. Phospholipid Nanoprobes for Tumor Targeting
Theranostic phospholipid nanoparticles: Co-loading indocyanine green (ICG) and phospholipid-encapsulated chemotherapeutics (e.g., cisplatin) constructs a "photothermal-chemotherapy" combined system. Near-infrared light (808 nm) irradiation triggers ICG photothermal effect (45–50°C) to disrupt tumor blood vessels while releasing drugs, achieving 92% tumor inhibition in mice—40% higher than single-drug therapy.
3. Long-Acting Phospholipid Carriers for Ocular Delivery
Phospholipid-hyaluronic acid composite gels: 5% lecithin-1% hyaluronic acid in-situ gels form semi-solid networks in tear fluid after eye drops. For glaucoma treatment, timolol ocular retention extends from 5 minutes (conventional eye drops) to 2 hours, maintaining intraocular pressure reduction for 24 hours and reducing daily administration from 3 to 1 times.
V. Special Application Scenarios of Biodegradable Phospholipids
1. Injectable In-Situ Forming Phospholipid Scaffolds
Thermosensitive phospholipid-poly(lactic-co-glycolic acid) (PLGA) composite systems: Liquid below 40°C, forming porous scaffolds at 37°C after injection. For bone defect repair, phospholipid scaffolds loaded with bone morphogenetic protein (BMP) enable slow BMP release (Last for 4 weeks), promoting 50% more new bone formation than pure PLGA scaffolds, with complete degradation within 3 months.
2. pH-Triggered Self-Assembling Phospholipid Gene Vectors
Histidine-modified phospholipids (His-PE): At acidic pH (6.0), protonated histidine promotes compact nanocomplexes (100 nm) with DNA; intracellular pH elevation to 7.4 dissociates complexes for DNA release. For gene therapy, this system achieves 2-fold higher transfection efficiency and 60% lower cytotoxicity than polyethyleneimine (PEI).
VI. Clinical Translation Challenges and Solutions
1. Quality Control for Scale Production
Batch stability of phospholipids: Fatty acid composition of natural phospholipids (e.g., soy lecithin) varies by origin, causing formulation performance fluctuations. Solutions:
Use synthetic phospholipids (e.g., DSPC, DPPC) with >99% purity and <2% batch-to-batch variation.
Develop "phospholipid-drug co-crystallization" technology, controlling crystal structure via X-ray diffraction to enhance formulation uniformity.
2. Stability Optimization for Long-Term Storage
Screening of lyoprotectants: Adding trehalose (5%) and mannitol (3%) during phospholipid liposome lyophilization increases glass transition temperature (Tg) from -20°C to +5°C. After 12-month storage at 4°C, liposome particle size increases <5% and drug retention rate >95% (vs. ~80% for traditional lyophilization).
3. Cost Control and Industrialization Paths
Modified utilization of low-cost phospholipids: Molecular distillation purifies crude phospholipids from waste egg yolk (purity increased from 60% to 90%), reducing costs by 40%. For common liposomes (e.g., amphotericin B liposomes), efficacy is equivalent to high-purity phospholipids.
VII. Frontier Exploration: Bionic Phospholipids and AI Design
1. Cell Membrane-Camouflaged Phospholipid Nanocarriers
Tumor cell membrane-coated phospholipid nanoparticles: Fusing membrane proteins from breast cancer cells (MCF-7) with phospholipids creates "Trojan horse" carriers. Animal experiments show 6.8-fold higher tumor accumulation, 3-fold faster intracellular doxorubicin release, and 70% reduced macrophage phagocytosis compared to unmodified nanoparticles.
2. AI-Assisted Phospholipid Formulation Design
Machine learning for predicting phospholipid-drug interactions: Neural network models input phospholipid structure parameters (e.g., fatty acid chain length, charge density) and drug properties (solubility, pKa) to predict optimal phospholipid ratios. AI-optimized antifungal formulations achieve drug loading from 12% to 25% with hemolysis rate <1% (traditional screening takes 3 months).
Conclusion
Innovative applications of phospholipids in drug formulations have evolved from simple drug loading to intelligent and bionic directions. Through molecular modification, composite system construction, and responsive design, they overcome bottlenecks of traditional formulations such as low bioavailability and poor targeting.


 CN
CN