Explore the therapeutic potential of phospholipids
Time:2025-05-28I. Pathological Basis of Neurodegenerative Diseases and the Role of Phospholipids
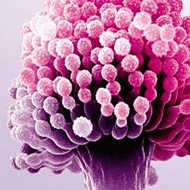
Core pathological features of neurodegenerative diseases (e.g., Alzheimer's disease AD, Parkinson's disease PD, Huntington's disease HD) include neuronal apoptosis, abnormal protein aggregation (e.g., β-amyloid Aβ in AD, α-synuclein in PD), and neuroinflammation. As the main component of neuronal membranes (accounting for 50%–60% of total brain lipids), phospholipid metabolic disorders are closely linked to neurodegeneration:
Compromised membrane structural integrity: Abnormal activity of phospholipid metabolic enzymes (e.g., phospholipase A2, sphingomyelinase) causes membrane phospholipid degradation, disrupting neuronal membrane fluidity and ion channel function, exacerbating calcium overload and oxidative stress.
Disordered signal transduction: Phospholipid-derived second messengers (e.g., diacylglycerol DAG, phosphatidylinositol trisphosphate PIP3) regulate neural survival and synaptic plasticity. Metabolic imbalance interferes with neurotrophic factor signaling pathways (e.g., PI3K-AKT pathway).
Promotion of protein aggregation: Abnormal phospholipid distribution (e.g., disordered sphingomyelin-cholesterol-enriched microdomains in synaptic membranes) induces oligomerization of Aβ and α-synuclein, forming toxic aggregates.
II. Therapeutic Potential of Phospholipids: From Mechanisms to Research Progress
1. Exogenous Phospholipid Supplementation: Repairing Neural Membranes and Synaptic Function
Clinical value of phosphatidylserine (PS)
PS, a specific phospholipid on the inner side of neuronal membranes, acts as an apoptotic signal upon spillover. Oral supplementation with naturally extracted PS (e.g., from soybeans or fish) crosses the blood-brain barrier, directly incorporating into neuronal membranes to restore fluidity and enhance synaptic vesicle neurotransmitter release. Clinical studies show PS improves memory scores (e.g., MMSE scale increase by 2–3 points) in AD patients, possibly by promoting cholinergic neuron survival and inhibiting Aβ deposition.
Phosphatidylcholine (PC) and acetylcholine synthesis
PC, a precursor of brain acetylcholine, increases synaptic acetylcholine concentration to alleviate cholinergic system decline in AD. Animal experiments show PC combined with donepezil (a cholinesterase inhibitor) synergistically improves learning and memory in APP/PS1 transgenic mice, reducing hippocampal Aβ plaque burden.
2. Regulating Phospholipid Metabolic Enzymes: Blocking Pathological Cascade Reactions
Inhibiting phospholipase A2 (PLA2) to reduce inflammation
Activation of cytosolic PLA2 (cPLA2) releases arachidonic acid, driving prostaglandin and leukotriene synthesis to exacerbate neuroinflammation. Small-molecule inhibitors (e.g., BEL208) specifically suppress cPLA2 activity, reducing microglial overactivation and protecting substantia nigra dopaminergic neurons in PD models.
Modulating sphingomyelinase (SMase) to improve protein aggregation
Excessive acidic SMase activation decomposes sphingomyelin into ceramide, promoting Aβ oligomerization. Antisense oligonucleotides (ASO) targeting SMase reduce brain ceramide levels in AD mice, decreasing hippocampal Aβ plaques by 40% and improving spatial memory.
3. Phospholipids as Drug Delivery Vectors: Enhancing Neuroprotectant Efficiency
Liposome-encapsulated neuroprotective drugs
Phospholipid-based liposomes encapsulate insoluble neuroprotectants (e.g., curcumin, resveratrol) for blood-brain barrier-targeted delivery. For example, curcumin liposomes achieve 8-fold higher brain concentration than free drugs in AD rats, significantly reducing Aβ-induced oxidative stress damage and improving hippocampal neuronal synaptic density.
pH-sensitive phospholipid nanoparticles
pH-responsive phospholipids (e.g., imidazole-containing phospholipids) construct nanoparticles that release nerve growth factor (NGF) in the acidic microenvironment of cerebral ischemic foci, specifically promoting neuronal regeneration in the peri-infarct zone. Animal experiments show this vector extends NGF brain retention to 72 hours, improving neurological function scores by 30% compared to free NGF.
4. Gene Therapy Targeting Phospholipid Metabolic Pathways
Correcting phospholipid synthase defects
Some neurodegenerative diseases relate to phospholipid synthase gene mutations (e.g., cholesterol 27-hydroxylase deficiency in cerebrotendinous xanthomatosis). Adeno-associated virus (AAV)-mediated delivery of phospholipid synthase genes (e.g., PCYT1A) restores phosphatidylcholine synthesis in liver and brain of mouse models, reversing myelin formation disorders.
III. Clinical Translation Challenges and Future Directions
1. Balance of Dosage and Safety
High-dose exogenous phospholipids (e.g., PS) may trigger platelet aggregation or gastrointestinal reactions, requiring optimized administration routes (e.g., intranasal delivery to reduce systemic exposure) and formulations (e.g., microencapsulated sustained release).
2. Individualized Treatment Strategies
Phospholipid metabolic abnormalities vary specifically among neurodegenerative diseases (e.g., PS reduction in AD, cardiolipin damage in PD), necessitating precise intervention via cerebrospinal fluid phospholipid profiling.
3. Combination Therapy Strategies
Combining phospholipid supplementation with drugs targeting protein aggregation (e.g., Aβ antibodies) may repair neural membranes while blocking pathological progression. Clinical trials show PS combined with lecanemab reduces brain atrophy rate by 15% in AD patients, outperforming monotherapy.
Conclusion
Phospholipids are not only the structural basis of nerve cells but also key nodes connecting multiple pathological links of neurodegeneration through their metabolic networks. From natural phospholipid supplementation to metabolic enzyme regulation and intelligent delivery system design, phospholipid-related therapies are progressively advancing from basic research to clinical application, providing an innovative and feasible new paradigm for preventing and treating neurodegenerative diseases.


 CN
CN