Phosphatidylserine and Intestinal flora
Time:2025-07-02Phosphatidylserine (PS), a phospholipid widely present in biological membranes, not only participates in maintaining cell structure and signal transduction but also its interaction with the intestinal microbiota has become a research hotspot in recent years. The bidirectional regulatory relationship between them plays an important role in maintaining intestinal homeostasis, metabolic balance, and immune function, with related studies gradually revealing its potential mechanisms and application value.
I. Metabolism and Transformation of Phosphatidylserine by Intestinal Microbiota
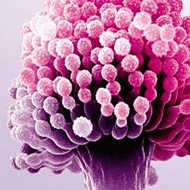
Intestinal microbiota directly participate in the decomposition and transformation of phosphatidylserine through the secretion of specific enzymes, affecting its bioavailability and downstream activity:
Phospholipase-mediated degradation: Some Gram-negative bacteria (such as Escherichia coli) and anaerobic bacteria (such as Bifidobacterium) can secrete phospholipases A2 and C, which catalyze the cleavage of ester bonds in phosphatidylserine molecules, releasing fatty acid chains and serine residues. Among them, serine can be used by the microbiota as a nitrogen source, while fatty acids (especially unsaturated fatty acids) may be further metabolized into short-chain fatty acids (SCFAs), indirectly regulating the intestinal environment.
Structural modification and reuse: Certain microbiota (such as Lactobacillus) can transfer the phosphate group in phosphatidylserine to their own cell membrane phospholipids through the phosphotransferase system, realizing the "reuse" of host-derived phosphatidylserine. This process may affect the stability of the microbiota's membrane structure and its adhesion ability to the intestinal epithelium.
Physiological activity of metabolites: Serine produced by the microbiota metabolism of phosphatidylserine can participate in the anabolic metabolism of intestinal mucosal cells, while SCFAs (such as butyric acid) can promote the proliferation of intestinal epithelial cells and enhance intestinal barrier function, forming a "microbiota-phosphatidylserine metabolites-host" synergistic regulatory network.
II. Regulation of Intestinal Microbiota Composition and Function by Phosphatidylserine
Phosphatidylserine can change the diversity and metabolic activity of intestinal microbiota through direct or indirect effects, thereby affecting microbiota balance:
Selectively promoting the proliferation of beneficial bacteria: In vitro experiments have shown that phosphatidylserine can act as a carbon source or signaling molecule to promote the growth of probiotics such as Bifidobacterium and Lactobacillus. For example, in a medium containing phosphatidylserine, the number of viable Bifidobacterium adolescentis is 2-3 times higher than that in the control group, and the mechanism may be related to the phospholipid components provided by PS enhancing the antioxidant capacity of the microbiota.
Inhibiting the excessive reproduction of conditional pathogens: The amphiphilic structure of phosphatidylserine may destroy the cell membrane integrity of certain pathogenic bacteria (such as Staphylococcus aureus and Salmonella), leading to the leakage of intracellular substances. Studies have found that supplementation with phosphatidylserine can reduce the abundance of Escherichia coli in the intestinal tract of mice and reduce the release of endotoxin (LPS), and this effect is more significant in the high-fat diet-induced microbiota imbalance model.
Regulating the metabolic function of microbiota: Phosphatidylserine can change the metabolic spectrum of microbiota by affecting their energy metabolism pathways (such as glycolysis and fatty acid synthesis). For example, phosphatidylserine intervention can increase the total amount of SCFAs produced by intestinal microbiota by 15%-20% and up-regulate the expression of enzyme genes related to tryptophan metabolism, indirectly affecting the synthesis of neurotransmitters in the host (such as serotonin).
III. Potential Impact of Interaction on Host Health
The bidirectional interaction between phosphatidylserine and intestinal microbiota is of great significance in various physiological and pathological processes:
Maintaining intestinal barrier and immune balance: Phosphatidylserine enhances intestinal mucosal tight junctions (such as the expression of occludin protein) and reduces intestinal permeability by promoting the proliferation of probiotics and the production of SCFAs; at the same time, its metabolites can regulate the activity of macrophages and dendritic cells, reducing excessive immune responses (such as the release of pro-inflammatory factors in inflammatory bowel disease). Animal experiments show that supplementation with phosphatidylserine can improve the imbalance of intestinal microbiota in colitis model mice, and inflammatory indicators (such as TNF-α and IL-6) are significantly down-regulated.
Linking metabolism and nerve function: Serine and SCFAs produced by the metabolism of phosphatidylserine by intestinal microbiota can affect the central nervous system through the "gut-brain axis". For example, SCFAs can act on the hypothalamus through the blood circulation to regulate appetite-related hormones (such as leptin); while serine, as a neurotransmitter precursor, may participate in the regulation of cognitive function, which provides new clues for the cross-system regulation of "phosphatidylserine-microbiota-brain health".
Potential value in disease intervention: In models of metabolic syndrome (such as obesity and diabetes), PS can improve insulin resistance by correcting microbiota imbalance (such as reducing the Firmicutes/Bacteroidetes ratio); in antibiotic-induced microbiota disorder, supplementation with PS can accelerate the recovery of microbiota diversity and reduce the risk of intestinal microbiota translocation.
IV. Research Challenges and Future Directions
There are still many unsolved problems in current research: For example, is the regulation of microbiota by phosphatidylserine strain-specific? Do phosphatidylserine from different sources (such as soybeans and egg yolks) lead to differences in interaction with microbiota due to differences in fatty acid composition? In addition, how phosphatidylserine and microbiota metabolites synergistically affect host immunity and metabolism still needs more in-depth mechanism research. In the future, it may be possible to achieve targeted intervention of related diseases through precise regulation of intestinal microbiota (such as probiotic combined with PS intervention), opening up new paths for the clinical application of phosphatidylserine.
The interaction between phosphatidylserine and intestinal microbiota is a complex dynamic network. Through metabolic coupling, structural interaction, and signal transmission, they jointly maintain the host's intestinal homeostasis and overall health. In-depth exploration of this field will provide new theoretical basis for nutritional intervention and disease prevention and treatment.


 CN
CN